Times have changed. 50 years ago, AUB was mainly treated by
surgical procedures, Dilatation and Curettage which stopped the bleeding temporarily
and also shed light on the endometrial curetting hyperplasia, precancerous changes
and endometrial cancer. Now there are many minor safe procedures, such as hysteroscopy,
removal of polyps, endometrial removal of small sub mucous fibroids others are
endometrial ablation, uterine artery embolization, (UAE), and off course Hysterectomy,
with or without bilateral removal of tubes and ovaries. These are for cancer,
pre-cancer treatment and major pelvic pathology e.g. large fibroids and ovarian
cysts. Removal of fibroids is often done as procedure called myomectomy. These
are sometimes treated by UAE so they shrink.
Endometrial ablation has come a long way since it started in the
nineties. Originally it was done by an electric instrument called Resectascope,
for which you required training and practice, as it could cause serious side
effects such as injury to the uterus and even the bowel.
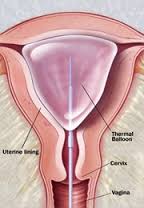
Now there is a large array of global endometrial ablation
(GEA) tools. The principal mainly applies to destroying the lining of the
uterus by radio frequency waves or by Cryo-freezing. Before we decide to ablate the endometrium,
we have to classify the cause of AUB. Making sure there is no intra uterine
pathology. A small fibroid 2-3cm can be dealt with GEA. Make sure there is no
cancer or pre-cancer pathology. It must be explained to the women that they
cannot have any babies. About 0.7 % of women
can conceive after GEA, but it is always disastrous. Some clinicians even do a
tubal ligation at the same time. After we have seen all the pros and cons of
GEA with the patient, do
an ultrasound to exclude
any uterine pathology, measure the uterine thickness, made sure there is no
pelvic infection, there is no scar in the uterus such as classical caesarean
section or myomectomy and cervix is not loose. Every surgeon and the hospital now
use the method they are competent with. GEA can be done soon after a period. Measure
the length of the uterine cavity. Put the device in, which can be of different
types, and once inside it they fit in with the uterine cavity. Radio frequency waves are passed for 90
seconds while we rotate the device to ablate the total cavity. Remove the
device after few seconds so that it cools down to avoid scaring of the cervix. There
can be a few serious problems such as uterine perforation. The patient can be
given pain relief for a few days.
The latest GEA was approved by FDA in 2015. It is called
Minerva. Minerva takes only 3-4 minutes. The device is inserted into the
uterine cavity. With this device, the radio frequency is delivered by ionized
Argon gas to create plasma. This is controlled by Impedance. The energy is
passed for 120seconds. The other
technique is microwaves; the advantage of microwaves is it can be used for a
bigger uterus. Just to name a few,
Genesys HTA, Cryo-ablation and heated free fluid and so on.
SURGICAL TREATMENT OF AUB FOR MYOMAS
Myomas are called leomyoma
in AUB in FIGO classification. The myomas affect about 50% of women in their life time. Many of these are asymptomatic, the main symptoms they cause are excessive or intermittent bleeding,
infertility, and pressure effects due to their size, frequency of urination,
constipation, walking difficulty, back ache and so on. If they are a
symptomatic there is no need to treat them. Minor problems happen with an
endometrial polyp. This can also cause post menopausal bleeding. It can be
easily treated on hysteroscopy by removing it. We always send it to pathology
as it rarely can be cancerous. The other problems are sub mucous fibroids they
can also be removed by hysteroscopy resection. If they are biggish and deep you
need a bit more training for this as, you may damage the uterus or rarely
adjoining organs. This helps with infertility treatment. A small sub mucous fibroid
less than 3 cms can be destroyed at the time of endometrial ablation
particularly by the microwave method; however you lose your fertility by GET.
The other method of treating these fibroids is to do what is
called uterine artery or fibroid embolization this procedure was first done in
1995. It is done by an interventional radiologist. It is best for fibroids
which are within the muscles of the uterus (Intramural). There is some dispute
about what is the biggest fibroid you can do it for. General agreement is if
the fibroid is bigger than 10cms in size do not do it. When it dies and sloughs
it causes problems. For this procedure
you are supposed to stop all your blood thinners, including aspirin and Nsaides
(pain relief drugs such as Ibobrufen), several days before. You are prepared
like any other operation. It is done under strict sterile conditions. You have
to stay in hospital overnight. The operation is performed in the groin on one
or both sides depending on the preference of the radiologist. It can be done
under local or general, anaesthesia depending on how brave you are.
A small cut is made over the femoral artery in the groin. A
small catheter size 1/8 of an inch in diameter is inserted and gradually guided
to the uterine artery, embolizing agents are injected. These particles are
about the size of sand, the catheter is than guided to the uterine artery on
the other side and injected. Some radiologists prefer to use the other side for
the uterine artery on the other side. UAE
should not be done if the woman is allergic to contrast media, she is pregnant,
has cancer, vascular or bleeding disorders, and recent or severe past pelvic
infections. This procedure gives
symptomatic relief in 83% within 6 months. Fibroids decrease in size from 40 to
70 %. Repeat treatment was required in
15 – 28 %. This intervention was done by
repeat UAE, myomectomy or hysterectomy. Women like to have UAE as it avoids too
much time off, major surgery, saves the uterus and saves fertility. The side
effects are it can cause infections, damage to ovarian blood supply, problems
with future pregnancy. One important side effect is post embolization syndrome.
Women run a low grade fever, pain, fatigue, nausea, vomiting and this peaks in
48 hours and then resolves in one week. If it fails to resolve we should look
for infection. Sometimes the material from the fibroids gets stuck in the
uterine cavity, and then the women require dilatation curettage for this
material to be removed.
The final surgical procedures are myomectomy this can be
assisted by reducing the size of the fibroids by GnRh analogues or
Ultrapristol. Then myomectomy can be performed by laparoscopy or normal laparatomy
depending on individual cases. Similarly Hysterectomy can be performed abdominally,
vaginal or laparoscopy assisted. It depends on the cases or surgeons preferences.
After myomectomy babies need to be delivered by caesarean section.
SUMMARY ABOUT AUB
The new FIGO classification of AUB and many current methods
of treatment have made a gynaecologists life very interesting. When you have a
case of AUB first classify it and then plan the treatment. Is it urgent, can we
manage by medical treatment or she requires surgical options? Always keep few things
in mind, patients age, her views, her needs, does she need contraception,
future pregnancy, does she have any medical problems, social situations, and
always respect her views with your line of treatment.