TURNER SYNDROME
One of the other causes of Primary Amenorrhoea is Turner Syndrome where one of the female sex chromosomes is missing.
They are usually of shorter stature, they usually appear in teenage years due to lack of developmental disorder.
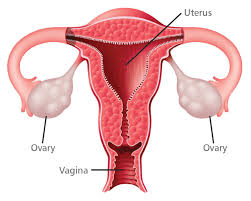
Some of these features are seen in this picture. They do have a uterus and maybe very small ovaries and the ovarian failure leads to Amenorrhoea. Diagnosis is made by clinical features, chromosomal analysis and ultrasound.
The current medical research in IVF can help some of these women to achieve a pregnancy with donor eggs.
I had two such patients that I looked after, they require hormone replacement to keep them healthy until the normal age of menopause.
The other common cause of primary amenorrhoea can be what we call Congenital Hyperplasia. This is due to a deficiency of a particular enzyme.
As a result of this the female baby becomes masculinised, it can happen in male foetuses as well, these babies are born with ambiguous genitalia but their chromosomes are normal.
These children have multiple problems with adrenal function. they need to be treated with paediatric endocrinologists.
Many other causes of primary amenorrhoea are tumours of the pituitary, failure of the female organs to develop and the failure of the organs to function.
Primary Amenorrhoea is a difficult complex disorder of infancy, child hood adolescence it needs to be treated by a group of experts including paediatricians and gynaecologists.
However don't forget the simple diagnosis of pregnancy should not be forgotten as a young girl with normal secondary sexual characters maybe pregnant although she has not had a period. The very first ovulation she can conceive. I have seen two such cases in my time. One of these girls was only twelve years of age and was brought to hospital at full term in labour.
This is just a very brief summary of Primary Amenorrhoea just to point out some important points;
1- When a baby is born with ambiguous sex it should be seen urgently by a paediatrician.
2- Babies suffering from Congenital Adrenal Hyperplasia (CAH) can be both male or female and their external sex is confusing, they also suffer from salt losing problems. They are life threatening and should be seen by a paediatrician.
3- The most common causes of Primary Amenorrhoea are Chromosomal Abnormalities - 50%
4- Hypothalamic Hypogonadism including Hypothalmic Amenorrhoea - 20%
5- Malformation of pelvic organs for example absence of the uterus, vaginal septum and imperforate hymen -20%
6- Pituitary disease , like tumours and infections -5%
7- Excessive weight loss like Anorexia Nervosa , obesity, psychiatric disorders and malnutrition -5%
The investigations are mainly;
1- Chromosomes, 2- Imaging, 3- Hormone Studies
Treatment depends on the cause mainly;
1- Lifestyle Factors, 2- Hormones, 3- Surgical Corrections
Finally don't forget pregnancy and take your child for medical advise as soon as possible.
We will talk about women's health issues and how to manage them correctly and be happy.
Monday, December 2, 2013
Monday, November 25, 2013
PRIMARY AMENORRHOEA
In this post today we will talk about Amenorrhoea(AMENO), this can be Primary or Secondary.
Primary Amenorrhoea a women has never had a period, but in secondary Amenorrhoea a period did start and then stopped.
(The word AMENORRHOEA is derived from the Greek A meaning NO and Men means month and Rhoea means flow.)
Today we will only discuss about Primary Amenorrhoea as the two topics together make a very long post.
To have normal periods you need a normal brain hypothalamus pituitary function as described in the menstrual cycle, and in addition to this you need a normal functioning ovary and a normal uterus, cervix and vagina. In addition to this there hormones should be co-ordinated and beside the ovary some other hormones also participate , such as the thyroid and general health also plays a role.
The abnormalities often start during foetal development due to chromosome and genetic defects.
The management of this problem should start at birth especially if the sex of the new born is ambiguous. These problems can be classified in various groups but I will just talk about random abnormalities. The domain of the treatment of these complicated abnormalities is in the hands of paediatric endocrinologists.
One of the interesting and not so rare conditions is called Androgen Insensitivity Syndrome is when a foetus who is genetically male(who has one X and Y chromosome) is resistant to male hormones(called Androgens). As a result the foetus develops the features of a female baby, and when this child grows up it looks like a very attractive female. She is tall, slim, attractive with normal breast development, flawless skin, however the female organs are not there except for a small depressed area for the vagina. These are called complete Androgen Insensitivity. Some of these may be incomplete and then they have features of both sexes. The testes often lie in the lower abdominal area , if that is the case they should be removed as they are prone to cancer. This individual always grows as a female and the diagnosis is made when they have no period(Primary Amenorrhoea). The diagnosis is confirmed by blood tests, and genetic testing which will be XY and ultrasound which will show no female organs. these women are treated by hormone replacement therapy , psychological counselling and removing of small testicles as already mentioned.
Most of these individuals suffering from AIS live as women and become involved in sports, modelling and working in the hospitality industry. In fact some of these women in these trades became very famous, and in fact until very recently if there was any doubt about there femineity there chromosomes were tested and if found to be XY they were removed from these sports, but since then it has been worked out that these androgens in these women do not work like normal androgens hence the name AIS, so this rule of ruling out AIS women with XY chromosomes from the sports has been removed.
In this day and age where we have the access and knowledge to all these tests that can be done, we should test a child when it is born should the genitalia be inconclusive.
One of the other situations that you may come across is a young girl who is between 14 and 16 years of age, has normal secondary sexual features but has not had a period, she should be investigated, they can often have pre menstrual symptoms, regular menstrual period pain but no period.
They often have an obstructive abnormality of the genital tract, meaning thereby their cervix, vagina and the hymen. They have a period but the blood cannot flow. If not released it gathers within the vagina, the uterus and the tubes whereby destroying them. The hymen abnormality is easily fixed by a cross incision on the area. If there is a vaginal septum it can be removed, the cervical stenosis is difficult to correct. If the uterus is absent and the ovaries are present the women do suffer pre menstrual symptoms but generally they do not have any complications, these days these women can have a surrogate pregnancy by using their egg and their partners sperm. If there were any problems with the vagina causing difficulty during sex it can be constructed.
We will continue this conversation in the next post.
Primary Amenorrhoea a women has never had a period, but in secondary Amenorrhoea a period did start and then stopped.
(The word AMENORRHOEA is derived from the Greek A meaning NO and Men means month and Rhoea means flow.)
Today we will only discuss about Primary Amenorrhoea as the two topics together make a very long post.
To have normal periods you need a normal brain hypothalamus pituitary function as described in the menstrual cycle, and in addition to this you need a normal functioning ovary and a normal uterus, cervix and vagina. In addition to this there hormones should be co-ordinated and beside the ovary some other hormones also participate , such as the thyroid and general health also plays a role.
The abnormalities often start during foetal development due to chromosome and genetic defects.
The management of this problem should start at birth especially if the sex of the new born is ambiguous. These problems can be classified in various groups but I will just talk about random abnormalities. The domain of the treatment of these complicated abnormalities is in the hands of paediatric endocrinologists.
One of the interesting and not so rare conditions is called Androgen Insensitivity Syndrome is when a foetus who is genetically male(who has one X and Y chromosome) is resistant to male hormones(called Androgens). As a result the foetus develops the features of a female baby, and when this child grows up it looks like a very attractive female. She is tall, slim, attractive with normal breast development, flawless skin, however the female organs are not there except for a small depressed area for the vagina. These are called complete Androgen Insensitivity. Some of these may be incomplete and then they have features of both sexes. The testes often lie in the lower abdominal area , if that is the case they should be removed as they are prone to cancer. This individual always grows as a female and the diagnosis is made when they have no period(Primary Amenorrhoea). The diagnosis is confirmed by blood tests, and genetic testing which will be XY and ultrasound which will show no female organs. these women are treated by hormone replacement therapy , psychological counselling and removing of small testicles as already mentioned.
Most of these individuals suffering from AIS live as women and become involved in sports, modelling and working in the hospitality industry. In fact some of these women in these trades became very famous, and in fact until very recently if there was any doubt about there femineity there chromosomes were tested and if found to be XY they were removed from these sports, but since then it has been worked out that these androgens in these women do not work like normal androgens hence the name AIS, so this rule of ruling out AIS women with XY chromosomes from the sports has been removed.
In this day and age where we have the access and knowledge to all these tests that can be done, we should test a child when it is born should the genitalia be inconclusive.
One of the other situations that you may come across is a young girl who is between 14 and 16 years of age, has normal secondary sexual features but has not had a period, she should be investigated, they can often have pre menstrual symptoms, regular menstrual period pain but no period.
They often have an obstructive abnormality of the genital tract, meaning thereby their cervix, vagina and the hymen. They have a period but the blood cannot flow. If not released it gathers within the vagina, the uterus and the tubes whereby destroying them. The hymen abnormality is easily fixed by a cross incision on the area. If there is a vaginal septum it can be removed, the cervical stenosis is difficult to correct. If the uterus is absent and the ovaries are present the women do suffer pre menstrual symptoms but generally they do not have any complications, these days these women can have a surrogate pregnancy by using their egg and their partners sperm. If there were any problems with the vagina causing difficulty during sex it can be constructed.
We will continue this conversation in the next post.
Thursday, November 7, 2013
PUBERTY
In this post we will talk about puberty. Puberty is the time when young girls undergo changes to their body, which matures them into being a woman, and from then on, they can carry on the most important human function of reproduction.
When I was a young girl there was no sex education in those days, and we never understood what puberty was. I remember one fine morning at the school that I had some vaginal bleeding and my best friend who was in my class who was slightly older than me and I went to her saying that I have got Tuberculosis down below. In those days the only cause of any bleeding we had known was Tuberculosis of the lung. She told me that it was menstruation and we discussed this in detail as she had started having her periods one year earlier. So you can see that the time of puberty varies in individuals depending on their general health, nutrition and lifestyle.
Therefore my sex education was derived from my classmate.
The boys also undergo maturation slightly later than girls, but in this post we will focus on girls only.
The word Puberty is derived from the Latin called PUBERATUM MATURATION.
As discuss in my previous post on menstruation we have certain glands in our body called endocrine
glands which produce chemicals that produce hormones. These hormones are linked to the site of the action via the blood stream. The main glands concerned in our maturation are Hypothalamus, Pituitary and Ovaries(Sex Glands in Females and Testes in the Male).
What happens at puberty under the direction of these hormones from the brain and the gonads, the breasts start to grow like little buds and then the second area of change is the appearance of pubic hair and axillary hair. In addition to the breasts and the hair their bodies start to change shape as years go by, they also have a special body odour. It is not uncommon for them to get changes in their skin and develop pimples.
In the genital area the mucosa of the vagina thickens and the labia minora changes. The vagina thickens and its PH changes. The eggs start to undergo maturation. The uterus enlarges and it achieves adult size and finally menstruation starts. Recently the hormone called Kisspeptin has been identified from the hypothalamus and this is supposed to kick start the menstrual cycle.
There can be some developmental abnormalities at puberty which we will discuss in future posts.
In summary the main hormones involved are from the hypothalamus,( Kisspeptin, GnRH,) Pituitary,(LH , FSH), Ovaries(Estradiol and Progesterone).
They have a self regulating control.
A small amount of testosterone comes from the ovary and another gland called Adrenal.
Adrenal is useful for the development of hair follicles.
We have also described these in the menstrual function.
When I was a young girl there was no sex education in those days, and we never understood what puberty was. I remember one fine morning at the school that I had some vaginal bleeding and my best friend who was in my class who was slightly older than me and I went to her saying that I have got Tuberculosis down below. In those days the only cause of any bleeding we had known was Tuberculosis of the lung. She told me that it was menstruation and we discussed this in detail as she had started having her periods one year earlier. So you can see that the time of puberty varies in individuals depending on their general health, nutrition and lifestyle.
Therefore my sex education was derived from my classmate.
The boys also undergo maturation slightly later than girls, but in this post we will focus on girls only.
The word Puberty is derived from the Latin called PUBERATUM MATURATION.
As discuss in my previous post on menstruation we have certain glands in our body called endocrine
glands which produce chemicals that produce hormones. These hormones are linked to the site of the action via the blood stream. The main glands concerned in our maturation are Hypothalamus, Pituitary and Ovaries(Sex Glands in Females and Testes in the Male).
What happens at puberty under the direction of these hormones from the brain and the gonads, the breasts start to grow like little buds and then the second area of change is the appearance of pubic hair and axillary hair. In addition to the breasts and the hair their bodies start to change shape as years go by, they also have a special body odour. It is not uncommon for them to get changes in their skin and develop pimples.
In the genital area the mucosa of the vagina thickens and the labia minora changes. The vagina thickens and its PH changes. The eggs start to undergo maturation. The uterus enlarges and it achieves adult size and finally menstruation starts. Recently the hormone called Kisspeptin has been identified from the hypothalamus and this is supposed to kick start the menstrual cycle.
There can be some developmental abnormalities at puberty which we will discuss in future posts.
In summary the main hormones involved are from the hypothalamus,( Kisspeptin, GnRH,) Pituitary,(LH , FSH), Ovaries(Estradiol and Progesterone).
They have a self regulating control.
A small amount of testosterone comes from the ovary and another gland called Adrenal.
Adrenal is useful for the development of hair follicles.
We have also described these in the menstrual function.
Monday, October 21, 2013
MENSTRUAL CYCLE AND MENSTRUATION
All living beings great and small have the main function of reproduction including humans.
The menstrual cycle is an integral part of this reproductive function. It is called menses and it is derived from the Latin word meaning monthly.
The main organs involved in this monthly cycle are Hypothalamus and Pituitary and they are located in the brain. The main female sex gland is called the ovary and it is located in the abdomen close to the uterus and the two tubes. The uterus is connected to the outside world by the cervix and the vagina. The chemicals produced by the hypothalamus and pituitary glands are called hormones which in turn act on the ovary which produces its own hormones. They help in the maturation of the egg and preparation of the uterus to receive the egg if fertilised.
If the pregnancy does not occur the prepared lining of the uterus is shed causing bleeding and this is called menstruation.Usually the menstruation starts around the ages of ten to fourteen years, and lasts for forty years in a women's life. The menstrual bleeding lasts three to seven days and blood loss is about 30 - 50 mls. The cycle usually varies between twenty-one to thirty five days.
It is only recently that we have started to understand what triggers the menstrual cycle.
They have found a new chemical called Kisspeptin which is supposed to trigger the hypothalamus to produce a hormone called GnRH.
GIIRH stimulates the pituitary to produces its hormones — follicle stimulating hormone (FSH) and luteinizing hormone (LH). These hormones ultimately cause the egg maturation and ovulation (the release of the mature egg from the ovarian follicle.
The menstrual cycle is an integral part of this reproductive function. It is called menses and it is derived from the Latin word meaning monthly.
The main organs involved in this monthly cycle are Hypothalamus and Pituitary and they are located in the brain. The main female sex gland is called the ovary and it is located in the abdomen close to the uterus and the two tubes. The uterus is connected to the outside world by the cervix and the vagina. The chemicals produced by the hypothalamus and pituitary glands are called hormones which in turn act on the ovary which produces its own hormones. They help in the maturation of the egg and preparation of the uterus to receive the egg if fertilised.
If the pregnancy does not occur the prepared lining of the uterus is shed causing bleeding and this is called menstruation.Usually the menstruation starts around the ages of ten to fourteen years, and lasts for forty years in a women's life. The menstrual bleeding lasts three to seven days and blood loss is about 30 - 50 mls. The cycle usually varies between twenty-one to thirty five days.
It is only recently that we have started to understand what triggers the menstrual cycle.
They have found a new chemical called Kisspeptin which is supposed to trigger the hypothalamus to produce a hormone called GnRH.
GIIRH stimulates the pituitary to produces its hormones — follicle stimulating hormone (FSH) and luteinizing hormone (LH). These hormones ultimately cause the egg maturation and ovulation (the release of the mature egg from the ovarian follicle.
Under
the influence of FSH, several primordial follicles start maturing but only one
becomes the dominant follicle for the cycle.
The growing egg produces oestrogens,
The oestrogens produced by the egg
stimulate a surge in the production of another hormone LH by the pituitary gland. This surge in
LH causes ovulation in the middle of the cycle, about fourteen days after the
follicle starts growing.
After the
egg is released, the remaining cells of the empty follicle turn into what is
called the corpus luteum (Latin for ‘yellow body’) which then produces the
second of the female hormones, progesterone, in the second half of the
menstrual cycle. In the first two weeks of the menstrual cycle, leading up to
ovulation, the oestrogens help the growth of the lining of the womb (the
endometrium). In the second two weeks, the progesterone matures or ripens this
lining.
If conception occurs, nutrition and
support is provided by this lining for the growing embryo. Progesterone levels
remain elevated, ensuring the stability of the womb lining, and enabling the
pregnancy to continue. However, if fertilisation does not occur, an abrupt fall
in oestrogen and progesterone levels takes place about 10—12 days after
ovulation. This drop in hormone levels destabilises the lining of the womb, which
is then shed as menstrual flow indicating the end of the ovarian cycle.
Menstruation
is a reassuring sign that the ovarian function is normal. A new cycle of
egg maturation begins.
At the time of menstruation other specific chemicals called prostaglandins are produced in the endometrium which may be responsible for period cramps, headaches, nausea and dizziness which can accompany a menstrual period.
Key points
1.
The ovary, the female sex
gland, is the main organ concerned with menstruation, reproduction, production
of the female hormones oestrogen and progesterone, and menopause.
2.
The ovary lies dormant from
birth to puberty and becomes dormant again at menopause, after four decades of
reproductive activity.
3.
It is now being researched what
biological catalysts activate, and then end, ovarian activity.
4. Oestrogens play the key
role in maintaining a woman’s health during the reproductive years.
5. There are many issues about menstruation that need to be discussed, such as;
A-Puberty, B-Amenorrhoea,(No Periods), C-Premenstrual tension(PMT),D-Painful Periods,
E-Heavy and Irregular Bleeding, F-Polycystic Ovaries, G-Contraception.
All these problems will be discussed in future posts.
Wednesday, October 2, 2013
REMAINING VULVAL DISORDERS
For the last few posts we have been focusing on various skin and mucous membrane problems that cause vulval pain ,discharge , discomfort and dyspareunia, most of these have already been elaborated on and I will discuss the remaining few today. It is very difficult to discuss all of them as many of them such as psoriasis, tinea, and lichen planus effect almost all parts of the body covered by skin and mucous membrane and they often come under the domain of a dermatologist.
One of the common group of inflammatory conditions of the vulva are called; 1-Lichen Planus, 2-Lichen Simplex Chronicus, 3- Lichen Sclerosis.
Lichen Planus is an erosive condition of the vulva which can affect both the vagina and the vulva, besides the genital area it can affect the scalp, hair and legs.
It has a reticulated purplish appearance which is very painful and uncomfortable. The diagnosis is confirmed by a biopsy and has a malignant potential, there is no definitive treatment, the patient needs reassurance, local emollients and steroids. Some people have tried testosterones. Recently cyclosporine are being tried.
The above picture is Lichen Simplex Chronicus.
This also causes itching and leads to chronic rubbing and scratching , this usually affects the labia Majora, Labia Minora, and Labia Crural Folds. The vagina is not involved, this can result from chronic infection , anxiety conditions such as Psoriasis, Eczema. The skin becomes thick and leathery as you can see in the above picture and brownish. So the treatment is again reassurance, tranquillisers, antihistamines, anti pruritic agents and corticosteroids. The cause of chronic anxiety or infection causing the itch also needs to be treated.
Lichen Sclerosis is a chronic inflammatory disorder of the skin affecting both genital and extra genital skin such as the armpit, neck and shoulder and sub memory fold below the breast.
It can occur at any age including children, usually if it occurs in young girls it goes away as they mature. Most often it occurs in post menopausal women. Again like other vulval skin problems it causes itching and pain. The skin gets thickened and causes adhesions. The local tissues are destroyed. We are not sure what causes this, but like Lichen Planus it is thought to be auto immune.
Autoimmunity is a process in which the body fails to recognize itself and therefore attacks its own cell and tissues.
The treatment consists of avoiding commercial body washes and antiseptic solutions. Washing with a freshly made saline solution of two teaspoons full of salt with one litre of water is very soothing.
You need to do this twice daily for several weeks, then repeat the wash as required.
Daily strong tropical steroids are required on your doctors advice.
Lichen Planus and Lichen Sclerosis both have a five percent cancer potential , therefore it is very important to have six monthly regular appointments with your gynaecologist.
The vulval conditions described above need patient education, psychological counselling, avoidance of commercial gimmicks, symptomatic treatment, saline washes, emollient's, corticosteroids, treatment for any inter current infections, ie: Thrush, (Candiasis) and above all regular check ups, and never treat yourself without correct diagnosis by a professional.
Bartholin's Cyst and Abscess
Bartholin gland is a small gland that lies in the entrance to the vagina and basically a small amount of fluid keeps the vagina moist which is useful during sexual intercourse. It has a small gland which carries the fluid to the vagina. If there is any infection the area, this little duct gets blocked and can cause a Bartolin's Cyst or Abcess. The important thing to know is that if it keeps happening it needs attention to exclude STI and often it requires drainage.
The above picture show the location of a swollen Bartholin Cyst and it's drainage.
Genital Herpes
Genital Herpes is caused by type one and type two herpes virus, initially not much attention was paid to this, but nowadays it is the most commonly transmitted disease. To prevent from yourself from getting herpes is to always use condoms, use suppressive viral therapy to protect your partner and avoid skin trauma by using silicone based lubricants.
The diagnosis is made by a swab test from the lesion, the blood tests are not so accurate. The initial attack of herpes is very painful. The treatment is anti viral drugs called Valtrex, Famvir and Zovirax.
The frequent occurrence can be treated by taking one tablet daily, this also protects transmission to the partner. It is very important to avoid herpes in the last few months of pregnancy as it can be dangerous to the newborn baby, and if the mother has an active rash on the vulva, the baby should be delivered by caesarean section.
Human Papilloma Virus is another virus which affects the female genital organs, particularly the cervix and the vagina and the vulva. The visible disease that is causes is the warts, otherwise it causes changes in the cervix which in the long term can lead to cervical cancer. To avoid cervical cancer that the smear test is implemented around the western world.
Please ensure that you have regular smear tests.
Another cause of vaginal discharge in post menopausal women is due to lack of oestrogens and it can be easily relieved by local oestrogen. However any women who suffers from irregular bleeding in the older age group must be investigated to exclude malignancy.
Often the vaginal discharge is due a foreign body and often this is a forgotten tampon.
The four tests which are useful for all these diagnoses is a cervical smear, swabs, biopsy and ultrasound.
You may have to read or research more to increase your knowledge on vulval vaginal infections.
And this is all from me on this topic.
In future posts we will continue our journey on Womens Health problems.
One of the common group of inflammatory conditions of the vulva are called; 1-Lichen Planus, 2-Lichen Simplex Chronicus, 3- Lichen Sclerosis.
Lichen Planus is an erosive condition of the vulva which can affect both the vagina and the vulva, besides the genital area it can affect the scalp, hair and legs.
It has a reticulated purplish appearance which is very painful and uncomfortable. The diagnosis is confirmed by a biopsy and has a malignant potential, there is no definitive treatment, the patient needs reassurance, local emollients and steroids. Some people have tried testosterones. Recently cyclosporine are being tried.
The above picture is Lichen Simplex Chronicus.
This also causes itching and leads to chronic rubbing and scratching , this usually affects the labia Majora, Labia Minora, and Labia Crural Folds. The vagina is not involved, this can result from chronic infection , anxiety conditions such as Psoriasis, Eczema. The skin becomes thick and leathery as you can see in the above picture and brownish. So the treatment is again reassurance, tranquillisers, antihistamines, anti pruritic agents and corticosteroids. The cause of chronic anxiety or infection causing the itch also needs to be treated.
Lichen Sclerosis is a chronic inflammatory disorder of the skin affecting both genital and extra genital skin such as the armpit, neck and shoulder and sub memory fold below the breast.
It can occur at any age including children, usually if it occurs in young girls it goes away as they mature. Most often it occurs in post menopausal women. Again like other vulval skin problems it causes itching and pain. The skin gets thickened and causes adhesions. The local tissues are destroyed. We are not sure what causes this, but like Lichen Planus it is thought to be auto immune.
Autoimmunity is a process in which the body fails to recognize itself and therefore attacks its own cell and tissues.
The treatment consists of avoiding commercial body washes and antiseptic solutions. Washing with a freshly made saline solution of two teaspoons full of salt with one litre of water is very soothing.
You need to do this twice daily for several weeks, then repeat the wash as required.
Daily strong tropical steroids are required on your doctors advice.
Lichen Planus and Lichen Sclerosis both have a five percent cancer potential , therefore it is very important to have six monthly regular appointments with your gynaecologist.
The vulval conditions described above need patient education, psychological counselling, avoidance of commercial gimmicks, symptomatic treatment, saline washes, emollient's, corticosteroids, treatment for any inter current infections, ie: Thrush, (Candiasis) and above all regular check ups, and never treat yourself without correct diagnosis by a professional.
Bartholin's Cyst and Abscess
Bartholin gland is a small gland that lies in the entrance to the vagina and basically a small amount of fluid keeps the vagina moist which is useful during sexual intercourse. It has a small gland which carries the fluid to the vagina. If there is any infection the area, this little duct gets blocked and can cause a Bartolin's Cyst or Abcess. The important thing to know is that if it keeps happening it needs attention to exclude STI and often it requires drainage.
Genital Herpes
Genital Herpes is caused by type one and type two herpes virus, initially not much attention was paid to this, but nowadays it is the most commonly transmitted disease. To prevent from yourself from getting herpes is to always use condoms, use suppressive viral therapy to protect your partner and avoid skin trauma by using silicone based lubricants.
The diagnosis is made by a swab test from the lesion, the blood tests are not so accurate. The initial attack of herpes is very painful. The treatment is anti viral drugs called Valtrex, Famvir and Zovirax.
The frequent occurrence can be treated by taking one tablet daily, this also protects transmission to the partner. It is very important to avoid herpes in the last few months of pregnancy as it can be dangerous to the newborn baby, and if the mother has an active rash on the vulva, the baby should be delivered by caesarean section.
Human Papilloma Virus is another virus which affects the female genital organs, particularly the cervix and the vagina and the vulva. The visible disease that is causes is the warts, otherwise it causes changes in the cervix which in the long term can lead to cervical cancer. To avoid cervical cancer that the smear test is implemented around the western world.
Please ensure that you have regular smear tests.
Another cause of vaginal discharge in post menopausal women is due to lack of oestrogens and it can be easily relieved by local oestrogen. However any women who suffers from irregular bleeding in the older age group must be investigated to exclude malignancy.
Often the vaginal discharge is due a foreign body and often this is a forgotten tampon.
The four tests which are useful for all these diagnoses is a cervical smear, swabs, biopsy and ultrasound.
You may have to read or research more to increase your knowledge on vulval vaginal infections.
And this is all from me on this topic.
In future posts we will continue our journey on Womens Health problems.
Monday, September 23, 2013
SNIPPETS OF INFORMATION ON VAGINAL DISCHARGE
1-Vaginal discharge is a variable subject what is normal for some women may be abnormal for others.
2-If you have a vaginal discharge do not start treatment without a diagnosis. What you may consider as just Thrush may even be malignancy. I have recently two such cases in older women. Post menopausal women generally do not get thrush until they are diabetic or using HRT.
3-When you have recurring Candidiasis it can be due to any oestrogens you may be taking, high oestrogen pill, poor diabetic control and due to another variety of Candida called Candida Glabrata.
For this you require stronger treatment called Intraconazole 200 mgs twice a day three times a week , then twice a week for four weeks.
There are other forms of treatment which you GP will advise you on.
4-When should you treat the male partner in recurring Candidiasis? The candida store itself in the seminal vessels and a culture of the semen should be done, and if positive the partner should be treated. The should also be treated if they have an infection of the penis and be given a local cream.
5-In cases of recurring candidiasis saline was once or twice a day is very comforting, it also helps with other inflammatory conditions , such as vestubulitis.
6-The other treatment could be , change the pill, control diabetes and general hygiene, not share garments with each other.
7-Boric acid gelatine pessaries can be used once or twice. If used frequently they can be toxic.
8-Vagina can be painted with Aqueous Gentian Violet 0.5 percent to 1.0 percent, once a week.
9-Last but not the least Depoprovera injections are often very useful to control Candidiasis.
One has to be careful if it is used long it can cause 1.0 percent loss of bone density thus causing osteoporosis.
10-Avoid local antiseptics, perfumes and commercial moisturisers. Anti histamines and Amytriptaline at bedtime is very useful. Chronic treatment of recurring Candidiasis can cause eczematic rash and local dermatitis.
So the take home message is , take the correct treatment after the correct diagnosis.
The next post will be on the remaining Vaginal Infections and Inflammations.
2-If you have a vaginal discharge do not start treatment without a diagnosis. What you may consider as just Thrush may even be malignancy. I have recently two such cases in older women. Post menopausal women generally do not get thrush until they are diabetic or using HRT.
3-When you have recurring Candidiasis it can be due to any oestrogens you may be taking, high oestrogen pill, poor diabetic control and due to another variety of Candida called Candida Glabrata.
For this you require stronger treatment called Intraconazole 200 mgs twice a day three times a week , then twice a week for four weeks.
There are other forms of treatment which you GP will advise you on.
4-When should you treat the male partner in recurring Candidiasis? The candida store itself in the seminal vessels and a culture of the semen should be done, and if positive the partner should be treated. The should also be treated if they have an infection of the penis and be given a local cream.
5-In cases of recurring candidiasis saline was once or twice a day is very comforting, it also helps with other inflammatory conditions , such as vestubulitis.
6-The other treatment could be , change the pill, control diabetes and general hygiene, not share garments with each other.
7-Boric acid gelatine pessaries can be used once or twice. If used frequently they can be toxic.
8-Vagina can be painted with Aqueous Gentian Violet 0.5 percent to 1.0 percent, once a week.
9-Last but not the least Depoprovera injections are often very useful to control Candidiasis.
One has to be careful if it is used long it can cause 1.0 percent loss of bone density thus causing osteoporosis.
10-Avoid local antiseptics, perfumes and commercial moisturisers. Anti histamines and Amytriptaline at bedtime is very useful. Chronic treatment of recurring Candidiasis can cause eczematic rash and local dermatitis.
So the take home message is , take the correct treatment after the correct diagnosis.
The next post will be on the remaining Vaginal Infections and Inflammations.
Monday, September 16, 2013
SUPERFICIAL VAGINAL INFECTIONS
While we are talking about Dyspareunia, let us complete the subject by talking about Superficial Vaginal Infections(SVI) and inflammatory conditions called Vulvar Dermatoses, they also cause Dyspareunia, Vulvo Vaginal Pruritus and Vaginal Discharge.
All women have vaginal discharge during their reproductive life, in varying amounts during their menstrual cycle. I wonder if any of you have ever thought what a great house keeping function this discharge does by keeping the vagina clean, by washing away the dead cells and infections.
This normal vaginal discharge comes from the glands located in cervix and the vagina.
There is increased discharge at appropriate times such as ovulation and sexual arousal.
It is very important to keep the personal vaginal hygiene up to date.
The question is where do these infections come from, some of the organisms are locally present and under conditions favourable to them , they start playing around and cause disease, the commonest of these is a fungus called Candida.
On other occasions the infections come after child birth, pelvic operations, sexual intercourse, unscientific use of antiseptics, scented soaps, bubble baths and washes and the list can go on.
The main discharge problems along with pain and pruritus are as follows;
1-Candidiasis,2-Bacterial Vaginosis,3-Trichomonas,4- Nabothian Follicles,5-Cytolitic Vaginosis,6-Streptococcal Vaginosis,7-Erosive Vaginitis,8-Atrophic Vaginitis,9-Chlamydia,10-Gonococcus,11-Foreign Body, 12-Malignancy.
We have already discussed Chlamydia and Gonococcus in our previous post on PID, its difficult to discuss all the above conditions, but we will discuss the commonest of these being Candidiasis, Bacterial Vaginosis, and Trichomonas.
VULVO VAGINAL CANDIDIASIS(VVC)
It is estimated that 50 to 70 percent of women of all ages during their reproductive life suffer from at least one episode of VVC.
They generally do not suffer prepuberty and postmenopausal, because Candida loves oestrogen and oestrogen milieu and during this period of life is absent or low.
The infection is caused by a variety of Candida Albicans, the other variety of Candida often found is called Candida Glabrata and this requires special and stronger treatment.
Vulva and Vagina are both involved but often not together. In diabetic women VVC is often very severe the area looks very inflamed and swollen and the infection spreads to the groin and perianal area.
The symptoms of VVC can be mild or severe and they include severe itching, and maybe pain on passing urine. The risk factors are pregnancy when the oestrogen level is high, use of antibiotics, diabetes, and HRT.
The diagnosis is easy considering the history, and examination which shows redness and white curdy discharge in the area.
There is a simple office microscopic test using saline and sodium hydroxide which shows fine filaments which is called pseudohyphae, this test also shows Trichomonas vaginalis -this organism will be readily recognisable by its characteristic movement.
Bacterial vaginosis -have a special cell, called a clue-cells.
We can also see the hormone status of the individual by looking at the vaginal cells. So this test gives a lot of information. Still it is best to send a vaginal swab, cervical cytology and STD test in high risk patients.
The treatment of VVC is to remove the risk factors, control diabetes and for the very first episode, local vaginal nystatin cream for one week, this can be used during pregnancy as well. It is important to clear candidiasis in pregnant women because it can be passed on to the baby at birth as an oral infection, subsequently the baby can pass it on to the mother during breast feeding.
If candidiasis persists we have to look for the reasons for persistence, I often do a glucose tolerance test to exclude diabetes, if they are on high dosage oestrogen pill, change the pill or use a different type of contraception. Depoprovera and Mirena are good alternatives. Mirena is a progesterone releasing intrauterine device. DPMA is an injectable progestron which is given by a IM injection of 150mg every three months.
Both these are good long term contraceptives and help in getting rid of chronic candidiasis.
Long term recurrence requires long term treatment, which is given over a period of six months.
1- Vaginal nystatin pessaries every night or alternate night for six months.
2-Oral flucanazole of 100mg twice weekly for six months.
3-Oral ketoconazole 200mg a day for six months. This is hepatoxic, so the liver needs to be tested every two to three months.
The vagina can be painted with gentian violet weekly for several weeks.
Once again the subject that we have just discussed needs more time and information and this will be followed up in our next post.
All women have vaginal discharge during their reproductive life, in varying amounts during their menstrual cycle. I wonder if any of you have ever thought what a great house keeping function this discharge does by keeping the vagina clean, by washing away the dead cells and infections.
This normal vaginal discharge comes from the glands located in cervix and the vagina.
There is increased discharge at appropriate times such as ovulation and sexual arousal.
It is very important to keep the personal vaginal hygiene up to date.
The question is where do these infections come from, some of the organisms are locally present and under conditions favourable to them , they start playing around and cause disease, the commonest of these is a fungus called Candida.
On other occasions the infections come after child birth, pelvic operations, sexual intercourse, unscientific use of antiseptics, scented soaps, bubble baths and washes and the list can go on.
The main discharge problems along with pain and pruritus are as follows;
1-Candidiasis,2-Bacterial Vaginosis,3-Trichomonas,4- Nabothian Follicles,5-Cytolitic Vaginosis,6-Streptococcal Vaginosis,7-Erosive Vaginitis,8-Atrophic Vaginitis,9-Chlamydia,10-Gonococcus,11-Foreign Body, 12-Malignancy.
We have already discussed Chlamydia and Gonococcus in our previous post on PID, its difficult to discuss all the above conditions, but we will discuss the commonest of these being Candidiasis, Bacterial Vaginosis, and Trichomonas.
VULVO VAGINAL CANDIDIASIS(VVC)
It is estimated that 50 to 70 percent of women of all ages during their reproductive life suffer from at least one episode of VVC.
They generally do not suffer prepuberty and postmenopausal, because Candida loves oestrogen and oestrogen milieu and during this period of life is absent or low.
The infection is caused by a variety of Candida Albicans, the other variety of Candida often found is called Candida Glabrata and this requires special and stronger treatment.
Vulva and Vagina are both involved but often not together. In diabetic women VVC is often very severe the area looks very inflamed and swollen and the infection spreads to the groin and perianal area.
The symptoms of VVC can be mild or severe and they include severe itching, and maybe pain on passing urine. The risk factors are pregnancy when the oestrogen level is high, use of antibiotics, diabetes, and HRT.
The diagnosis is easy considering the history, and examination which shows redness and white curdy discharge in the area.
There is a simple office microscopic test using saline and sodium hydroxide which shows fine filaments which is called pseudohyphae, this test also shows Trichomonas vaginalis -this organism will be readily recognisable by its characteristic movement.
Bacterial vaginosis -have a special cell, called a clue-cells.
We can also see the hormone status of the individual by looking at the vaginal cells. So this test gives a lot of information. Still it is best to send a vaginal swab, cervical cytology and STD test in high risk patients.
The treatment of VVC is to remove the risk factors, control diabetes and for the very first episode, local vaginal nystatin cream for one week, this can be used during pregnancy as well. It is important to clear candidiasis in pregnant women because it can be passed on to the baby at birth as an oral infection, subsequently the baby can pass it on to the mother during breast feeding.
If candidiasis persists we have to look for the reasons for persistence, I often do a glucose tolerance test to exclude diabetes, if they are on high dosage oestrogen pill, change the pill or use a different type of contraception. Depoprovera and Mirena are good alternatives. Mirena is a progesterone releasing intrauterine device. DPMA is an injectable progestron which is given by a IM injection of 150mg every three months.
Both these are good long term contraceptives and help in getting rid of chronic candidiasis.
Long term recurrence requires long term treatment, which is given over a period of six months.
1- Vaginal nystatin pessaries every night or alternate night for six months.
2-Oral flucanazole of 100mg twice weekly for six months.
3-Oral ketoconazole 200mg a day for six months. This is hepatoxic, so the liver needs to be tested every two to three months.
The vagina can be painted with gentian violet weekly for several weeks.
Once again the subject that we have just discussed needs more time and information and this will be followed up in our next post.
Monday, August 12, 2013
PELVIC INFLAMMATORY DISEASE
Michelle aged 33 came to see me complaining of infertility, meaning that she was unable to conceive within the last fourteen months, she was advised that the reason for this is damage to her tubes.
She was not aware of any illnesses that may have caused this, my immediate reaction was that she probably had very mild pelvic inflammatory disease at college, which often can be silent and can cause tubal damage.
Technically (PID) is a term used to express infection of the uterus , tubes and ovaries, which often results in long term damage of the tubes, adhesions and infertility. This causes chronic Dyspareunia, pelvic pain and backache.
I feel that the infections of the cervix, vagina and vulva should also be included as PID.
The main reason for PID in younger people is by sexually transmitted infections, the typical person having these problems is a young women having periods and sexually active.
The other causes of PID are infections during an abortion or miscarriage, intrauterine devices and blood born diseases, such as Tuberculosis which is relatively rare in the western world.
The infecting organisms, Chlamydia Trachomatis, Neisseria Gonorrhoea are sexually transmitted bacteria which can cause asymptomatic infection or very serious disease.
Other sexually transmitted disease are Herpes Virus, which causes changes in the cervix called cervical dysplasia and this if progressed can lead to cervical cancer, this does not cause an infection of the uterus, tubes or the ovaries or in other words the internal organs. Trichomonas Vaginalis which is not a bacteria but is a protozoa. (A type of infecting organism) which is also sexually transmitted. It mainly affects the vagina causing smelly discharge and itching.
Other organisms that live happily in that region are likely to cause infection such as streptococcus Ecoli.
The diagnosis in Michelle's case was made by laparoscopy when on testing the tubes they were found to be blocked and convoluted. This can also be tested by a radiological test , but laparoscopy gives better information as regards adhesions in the pelvis. So obviously she must have had a silent episode of PID in her younger years. By the frequent nature of silent STD's amongst young women it was assumed that this was also an STD. A cervical swab was performed for Chlamydia and Gonorrhoea but as expected it was negative for both. Besides the swabs, laparoscopy and ultrasound often prior to laparoscopy and blood tests are also performed. The blood test which can give us an idea of an active infection is called CRP.
When you have mild symptoms of pelvic pain, altered menstrual function, pain on intercourse, please do not ignore them and do not run the risk of silent PID, as we have learnt in Michelle's case the long term consequences can be permanent.
Thanks to modern assisted reproductive technology, Michelle was helped to have a healthy baby.
When a women presents with pelvic pain, altered bleeding, there are many other conditions that have to be kept in mind. One of the most important is an Ectopic Pregnancy. The current pregnancy tests are extremely accurate, and if it is a positive result it's highly possible that the women has an Ectopic Pregnancy , this could be the result of a past or present PID.
Other diagnoses that should be remembered are appendicitis, septic abortion, haemorrhagic ruptured ovarian cyst, twisted ovary, degenerating fibroid and enteritis.
Clinical history, pelvic examination, blood test, pregnancy test, ultrasound, swab test, and finally laparoscopy will give us the diagnosis.
The treatment depends on the cause and in PID multiple antibiotic therapy is recommended as often we are unable to grow the infecting organism in PID.
It is very important to clear the PID as the long term consequences are serious and dangerous, as already mentioned it can cause infertility, chronic PID, chronic adhesions even affecting the liver, Ectopic Pregnancy, and even death in some situations.
PID is a serious disease and every attempt should be made to treat it early on very minor symptoms, such as vaginal discharge, pain and bleeding.
The most important thing is to have regular medical check ups if you are sexually active, and should you have a new sexual partner have him tested for STD's.
The second thing is do not take over the counter medicines for vaginal discharge or itch, without a proper diagnosis. All that itches is not thrush.
I have seen a women in her seventies who was treating herself for thrush and in fact it was vulval carcinoma.
Post menopausal women do not get thrush unless they are diabetic or taking excessive HRT.
Although women who are post menopausal, are not so prone to PID, but occasionally they get a collection of pus inside the uterus called pyometra, this needs treatment.
The moral of the story is do not consider vaginal discharge insignificant, have it seen to, and do not treat yourself.
We will discuss the superficial pelvic infections on my next post.
She was not aware of any illnesses that may have caused this, my immediate reaction was that she probably had very mild pelvic inflammatory disease at college, which often can be silent and can cause tubal damage.
Technically (PID) is a term used to express infection of the uterus , tubes and ovaries, which often results in long term damage of the tubes, adhesions and infertility. This causes chronic Dyspareunia, pelvic pain and backache.
I feel that the infections of the cervix, vagina and vulva should also be included as PID.
The main reason for PID in younger people is by sexually transmitted infections, the typical person having these problems is a young women having periods and sexually active.
The other causes of PID are infections during an abortion or miscarriage, intrauterine devices and blood born diseases, such as Tuberculosis which is relatively rare in the western world.
The infecting organisms, Chlamydia Trachomatis, Neisseria Gonorrhoea are sexually transmitted bacteria which can cause asymptomatic infection or very serious disease.
Other sexually transmitted disease are Herpes Virus, which causes changes in the cervix called cervical dysplasia and this if progressed can lead to cervical cancer, this does not cause an infection of the uterus, tubes or the ovaries or in other words the internal organs. Trichomonas Vaginalis which is not a bacteria but is a protozoa. (A type of infecting organism) which is also sexually transmitted. It mainly affects the vagina causing smelly discharge and itching.
Other organisms that live happily in that region are likely to cause infection such as streptococcus Ecoli.
The diagnosis in Michelle's case was made by laparoscopy when on testing the tubes they were found to be blocked and convoluted. This can also be tested by a radiological test , but laparoscopy gives better information as regards adhesions in the pelvis. So obviously she must have had a silent episode of PID in her younger years. By the frequent nature of silent STD's amongst young women it was assumed that this was also an STD. A cervical swab was performed for Chlamydia and Gonorrhoea but as expected it was negative for both. Besides the swabs, laparoscopy and ultrasound often prior to laparoscopy and blood tests are also performed. The blood test which can give us an idea of an active infection is called CRP.
When you have mild symptoms of pelvic pain, altered menstrual function, pain on intercourse, please do not ignore them and do not run the risk of silent PID, as we have learnt in Michelle's case the long term consequences can be permanent.
Thanks to modern assisted reproductive technology, Michelle was helped to have a healthy baby.
When a women presents with pelvic pain, altered bleeding, there are many other conditions that have to be kept in mind. One of the most important is an Ectopic Pregnancy. The current pregnancy tests are extremely accurate, and if it is a positive result it's highly possible that the women has an Ectopic Pregnancy , this could be the result of a past or present PID.
Other diagnoses that should be remembered are appendicitis, septic abortion, haemorrhagic ruptured ovarian cyst, twisted ovary, degenerating fibroid and enteritis.
Clinical history, pelvic examination, blood test, pregnancy test, ultrasound, swab test, and finally laparoscopy will give us the diagnosis.
The treatment depends on the cause and in PID multiple antibiotic therapy is recommended as often we are unable to grow the infecting organism in PID.
It is very important to clear the PID as the long term consequences are serious and dangerous, as already mentioned it can cause infertility, chronic PID, chronic adhesions even affecting the liver, Ectopic Pregnancy, and even death in some situations.
PID is a serious disease and every attempt should be made to treat it early on very minor symptoms, such as vaginal discharge, pain and bleeding.
The most important thing is to have regular medical check ups if you are sexually active, and should you have a new sexual partner have him tested for STD's.
The second thing is do not take over the counter medicines for vaginal discharge or itch, without a proper diagnosis. All that itches is not thrush.
I have seen a women in her seventies who was treating herself for thrush and in fact it was vulval carcinoma.
Post menopausal women do not get thrush unless they are diabetic or taking excessive HRT.
Although women who are post menopausal, are not so prone to PID, but occasionally they get a collection of pus inside the uterus called pyometra, this needs treatment.
The moral of the story is do not consider vaginal discharge insignificant, have it seen to, and do not treat yourself.
We will discuss the superficial pelvic infections on my next post.
Monday, July 22, 2013
RESIDUAL OVARY OR OVARIAN REMENANT SYNDROME
Stephanie aged 48, came to see me with severe Dyspareunia.
She had a Hysterectomy with the ovaries conserved six years ago, and for the last two years this pain was gradually increasing, she had seen two other clinicians who had advised her to use local oestrogen cream and maybe change coital position. This treatment did not help her.
When I saw her on examination her vagina was not dry and she was tender on both sides where her ovaries were supposed to be located, and on moving the vaginal apex she felt pain.
My diagnosis was immediately clear that it was what we call Residual Ovary Syndrome(ROS).
A pelvic ultrasound was performed , this did not show any disease of the ovaries. I offered Stephanie Bilateral Salpingo-oophorectomy.(Removal of both tubes and ovaries), followed by hormone replacement.
Stephanie agreed to this and was a million dollars after treatment.
ROS is a condition which is not often thought of and many times women are older and are reluctant to discuss the condition of dyspareunia. Even if they do, they are more often offered local treatment.
ROS has been found to happen in two to three percent of cases after hysterectomy when the ovaries have been conserved. Usually three percent of these are found to be cancerous. Arguments continue if the ovaries should be removed with each hysterectomy. The general consensus of opinion is that if a woman is older than 45, removal should be considered depending on the woman's risk factors if she takes HRT for a long time. These are family history of breast cancer, stroke, deep venous thrombosis and heart disease.
If there is a family history of ovarian cancer it can become a bit tricky.
The final decision should be made by the woman depending on her individual choice.
ROS is characterised by pelvic pain, pelvic mass and dyspareunia. When a woman presents with one or more of these symptoms a clinical examination should be performed. An ultrasound examination often gives a diagnosis if there is an ovarian cyst or a mass. Further evaluation can give an idea if there is any suggestion of malignancy. Often a CT and a MRI is performed which can help the diagnosis in difficult cases. Sometimes these cysts arise from the peritoneum, which is a membrane that covers the inside of our belly.
The blood test for the patients general health and hormone studies to assess the ovarian function are useful. There is a test called CA125 which is a screening test for cancer, if it shows a low value, we can assume that there is no cancer.
If we have excluded ovarian cancer with certainty by our tests, then the treatment can be one of the following;
1- Can be medical by hormones-Depo-Provera, GnRH Analogues, both these hormones suppress the ovaries and give temporary relief.
2- Aspiration of the cyst on the ovary, this fluid is sent for testing to exclude any cancer cells. This is also temporary, but it can be repeated more than once.
3- Radiation of the ovaries will stop them making physiological cysts.
4- The final and definitive treatment is by the removal of the ovaries or the remnants. This can be done either by key hole surgery or open surgery. This can be a difficult surgery because the adhesion's form around the ovaries, involving the bowel and ureter which can be damaged in the process.
In the first place these remnants are left behind because the initial operation was difficult due to pelvic adhesion's as a result of endometriosis and pelvic infections.
This has to be followed by supervised hormone replacement.
5 If there is any doubt about the ovarian mass or cyst being cancerous have it removed.
In summarising do not ignore post hysterectomy pelvic pain if you have one or both of your ovaries, have the necessary investigations and treatment. Do not be frightened of Hormone Replacement Treatment, it can make your life very comfortable if given under proper supervision.
She had a Hysterectomy with the ovaries conserved six years ago, and for the last two years this pain was gradually increasing, she had seen two other clinicians who had advised her to use local oestrogen cream and maybe change coital position. This treatment did not help her.
When I saw her on examination her vagina was not dry and she was tender on both sides where her ovaries were supposed to be located, and on moving the vaginal apex she felt pain.
My diagnosis was immediately clear that it was what we call Residual Ovary Syndrome(ROS).
A pelvic ultrasound was performed , this did not show any disease of the ovaries. I offered Stephanie Bilateral Salpingo-oophorectomy.(Removal of both tubes and ovaries), followed by hormone replacement.
Stephanie agreed to this and was a million dollars after treatment.
ROS is a condition which is not often thought of and many times women are older and are reluctant to discuss the condition of dyspareunia. Even if they do, they are more often offered local treatment.
ROS has been found to happen in two to three percent of cases after hysterectomy when the ovaries have been conserved. Usually three percent of these are found to be cancerous. Arguments continue if the ovaries should be removed with each hysterectomy. The general consensus of opinion is that if a woman is older than 45, removal should be considered depending on the woman's risk factors if she takes HRT for a long time. These are family history of breast cancer, stroke, deep venous thrombosis and heart disease.
If there is a family history of ovarian cancer it can become a bit tricky.
The final decision should be made by the woman depending on her individual choice.
ROS is characterised by pelvic pain, pelvic mass and dyspareunia. When a woman presents with one or more of these symptoms a clinical examination should be performed. An ultrasound examination often gives a diagnosis if there is an ovarian cyst or a mass. Further evaluation can give an idea if there is any suggestion of malignancy. Often a CT and a MRI is performed which can help the diagnosis in difficult cases. Sometimes these cysts arise from the peritoneum, which is a membrane that covers the inside of our belly.
The blood test for the patients general health and hormone studies to assess the ovarian function are useful. There is a test called CA125 which is a screening test for cancer, if it shows a low value, we can assume that there is no cancer.
If we have excluded ovarian cancer with certainty by our tests, then the treatment can be one of the following;
1- Can be medical by hormones-Depo-Provera, GnRH Analogues, both these hormones suppress the ovaries and give temporary relief.
2- Aspiration of the cyst on the ovary, this fluid is sent for testing to exclude any cancer cells. This is also temporary, but it can be repeated more than once.
3- Radiation of the ovaries will stop them making physiological cysts.
4- The final and definitive treatment is by the removal of the ovaries or the remnants. This can be done either by key hole surgery or open surgery. This can be a difficult surgery because the adhesion's form around the ovaries, involving the bowel and ureter which can be damaged in the process.
In the first place these remnants are left behind because the initial operation was difficult due to pelvic adhesion's as a result of endometriosis and pelvic infections.
This has to be followed by supervised hormone replacement.
5 If there is any doubt about the ovarian mass or cyst being cancerous have it removed.
In summarising do not ignore post hysterectomy pelvic pain if you have one or both of your ovaries, have the necessary investigations and treatment. Do not be frightened of Hormone Replacement Treatment, it can make your life very comfortable if given under proper supervision.
Monday, July 15, 2013
ADNEXAL CAUSES OF DYSPAREUNIA
Mary went to see her Gynaecologist all upset to find that she had a cyst on the left ovary.
Recently there has been a fair bit of talk about Ovarian Cancer, however all the cysts are not cancer, there are lots of different types of cysts on the ovaries which are harmless, particularly in young women.
What are ovaries?, they are the main sex organs in the female who along with the uterus perform the human reproductive function. Ovaries along with their tubes are referred as Adnexa.
The above diagram shows the maturation of the egg.
These amazing organs lay dormant until puberty then they become active for 30 to 40 years of a women's reproductive life and then they stop again and this is then called Menopause.
Scientists are still trying to study what suddenly brings on puberty.
I think that they are close to solving this puzzle.
Scattered in the ovary are millions of immature eggs. these are called primordial follicles.
In the foetal ovary there are millions of these , at puberty there are about four hundred thousand, they gradually mature into eggs, the rest dry up and at menopause we run out of them.
As the primordial follicle matures it makes a cyst that is a cavity full of fluid, this has hormones and this is called follicle cyst. This is one of the common cause of pelvic pain, especially in the midcycle when it is growing and releases the egg. Sometimes it overgrows and causes a follicular cyst, which causes pain. After the follicle ruptures it forms another cyst, which is called corpus luteum cyst and when picked up by ultrasound , both these cysts cause anxiety in women, however they are not cancerous. We call them physiological cysts as they are the result of cyclical ovarian function.
They are causing symptoms , such as acute pain, haemorrhage, torsion(twisted), grow bigger than five centimetres and do not resolve by themselves, then they require surgical removal which can be done by key hole surgery. It is often best not to disturb the corpus luteum cyst as it can bleed during surgery and subsequently causes scar tissue.
There are many different types of ovarian cysts and we will discuss these in another post, and most of these are often pain free, unless touched during intercourse.
The other Adnexal Pathology that causes Acute Dyspareunia is an ectopic pregnancy , which means pregnancy in the tube. The diagnosis is made by a pregnancy test and an ultrasound. Again urgent treatment is recommended.
The other ovarian conditions related to acute pain not necessarily related to dyspareunia are torsion of the ovary, rupture of an ovarian cyst. All these conditions require urgent medical attention.
Recently there has been a fair bit of talk about Ovarian Cancer, however all the cysts are not cancer, there are lots of different types of cysts on the ovaries which are harmless, particularly in young women.
What are ovaries?, they are the main sex organs in the female who along with the uterus perform the human reproductive function. Ovaries along with their tubes are referred as Adnexa.
The above diagram shows the maturation of the egg.
These amazing organs lay dormant until puberty then they become active for 30 to 40 years of a women's reproductive life and then they stop again and this is then called Menopause.
Scientists are still trying to study what suddenly brings on puberty.
I think that they are close to solving this puzzle.
Scattered in the ovary are millions of immature eggs. these are called primordial follicles.
In the foetal ovary there are millions of these , at puberty there are about four hundred thousand, they gradually mature into eggs, the rest dry up and at menopause we run out of them.
As the primordial follicle matures it makes a cyst that is a cavity full of fluid, this has hormones and this is called follicle cyst. This is one of the common cause of pelvic pain, especially in the midcycle when it is growing and releases the egg. Sometimes it overgrows and causes a follicular cyst, which causes pain. After the follicle ruptures it forms another cyst, which is called corpus luteum cyst and when picked up by ultrasound , both these cysts cause anxiety in women, however they are not cancerous. We call them physiological cysts as they are the result of cyclical ovarian function.
They are causing symptoms , such as acute pain, haemorrhage, torsion(twisted), grow bigger than five centimetres and do not resolve by themselves, then they require surgical removal which can be done by key hole surgery. It is often best not to disturb the corpus luteum cyst as it can bleed during surgery and subsequently causes scar tissue.
There are many different types of ovarian cysts and we will discuss these in another post, and most of these are often pain free, unless touched during intercourse.
The other Adnexal Pathology that causes Acute Dyspareunia is an ectopic pregnancy , which means pregnancy in the tube. The diagnosis is made by a pregnancy test and an ultrasound. Again urgent treatment is recommended.
The other ovarian conditions related to acute pain not necessarily related to dyspareunia are torsion of the ovary, rupture of an ovarian cyst. All these conditions require urgent medical attention.
Wednesday, July 3, 2013
PELVIC CONGESTION SYNDROME
In our previous posts we enumerated some causes of Deep Dyspareunia and we are endeavouring to cover all these causes, in a little bit more detail but not in the order that we posted previously.
In this post we will focus on Pelvic Congestion Syndrome (PCS). Nearly 30 percent of women suffer from this condition in their lifetime. The top age group is between 20 to 45 years of age. It is caused by , varicose veins in the pelvis around the uterus and ovaries, similar to varicose veins in the legs.
It is not understood if there is a genetic factor or anatomical factor in the formation of the veins.
The women suffer from chronic lower abdominal discomfort, backache and pain on intercourse, it gets worse at the end of the day and after sex.
The other symptoms they suffer is heavy painful periods, vaginal discharge, bladder discomfort and mood swings.
It usually happens after child birth, with the hormone changes and weight gain during pregnancy, which puts pressure on the ovarian veins and the blood flow is impeded. High levels of oestrogen during pregnancy dilates the veins, further contributing to the problem. With each pregnancy over time the uterus enlarges, the lining of the uterus becomes thicker and often the uterus falls backwards(this is called Retroversion), this further adds to the problem of dyspareunia, the periods become heavier and painful.
The diagnosis of PCS is difficult because there are nearly twenty other conditions which cause the complex chronic backache, heavy and painful periods and dyspareunia.
About twenty years ago we offered them medical treatment, often followed by hysterectomy.This did not really help the women and their symptoms continued. The removal of the ovaries was more helpful, but then the problem was of sudden surgical menopause and hormone replacement was required. And we replaced one problem with another.
Luckily we have learnt a lot more about PCS and are able to help the vast majority of women.
Most of the clinicians being aware of the problem, try to tackle it in the modern way.
The history and clinical examination helps us to exclude many other conditions, such as large fibroids and ovarian cysts.
The diagnosis is of exclusion of other causes. An ultrasound examination is useful to exclude other pathology, but often it does not highlight the veins because it is carried out in a supine position. The new colour ultrasound is useful if available to show us the uterine congestion.
CT and MRI is useful however CT is more invasive as we have to use injection of dyes to highlight the problem and the patient is exposed to radiation.
Venogram is most helpful in making a diagnosis, as it is not too drastic. Only, it has to be done by a special radiologist at a specialist centre.
They can inject the veins with sclerosing agents to block them and they can put little clips inside the veins so that the backward blood flow is stopped. This simple treatment of embolization gives women satisfactory results for several years. The very latest diagnostic and therapeutic technology to manage this condition, treating it effectively with a minimally invasive outpatient procedure.
These pictures show the vascular uterus on colour ultrasound, a venogram of pelvic organs with venous congestion, and post treatment ,left ovarian vein.
For those women who cannot avail themselves of the most current and remarkable treatment for PCS
the old medical treatment still helps.
This consists of pain relief by non steroidal antinflammatory medications, oral contraceptive pills, and drugs to suppress the ovaries. Some people believe in Acupuncture, Homeopathic and Osteopathy. Surely all this can be tried with adequate rest and counselling.
In the next post we will talk about Adnexal Pathology (Tubes and Ovaries)
In this post we will focus on Pelvic Congestion Syndrome (PCS). Nearly 30 percent of women suffer from this condition in their lifetime. The top age group is between 20 to 45 years of age. It is caused by , varicose veins in the pelvis around the uterus and ovaries, similar to varicose veins in the legs.
It is not understood if there is a genetic factor or anatomical factor in the formation of the veins.
The women suffer from chronic lower abdominal discomfort, backache and pain on intercourse, it gets worse at the end of the day and after sex.
The other symptoms they suffer is heavy painful periods, vaginal discharge, bladder discomfort and mood swings.
It usually happens after child birth, with the hormone changes and weight gain during pregnancy, which puts pressure on the ovarian veins and the blood flow is impeded. High levels of oestrogen during pregnancy dilates the veins, further contributing to the problem. With each pregnancy over time the uterus enlarges, the lining of the uterus becomes thicker and often the uterus falls backwards(this is called Retroversion), this further adds to the problem of dyspareunia, the periods become heavier and painful.
The diagnosis of PCS is difficult because there are nearly twenty other conditions which cause the complex chronic backache, heavy and painful periods and dyspareunia.
About twenty years ago we offered them medical treatment, often followed by hysterectomy.This did not really help the women and their symptoms continued. The removal of the ovaries was more helpful, but then the problem was of sudden surgical menopause and hormone replacement was required. And we replaced one problem with another.
Luckily we have learnt a lot more about PCS and are able to help the vast majority of women.
Most of the clinicians being aware of the problem, try to tackle it in the modern way.
The history and clinical examination helps us to exclude many other conditions, such as large fibroids and ovarian cysts.
The diagnosis is of exclusion of other causes. An ultrasound examination is useful to exclude other pathology, but often it does not highlight the veins because it is carried out in a supine position. The new colour ultrasound is useful if available to show us the uterine congestion.
CT and MRI is useful however CT is more invasive as we have to use injection of dyes to highlight the problem and the patient is exposed to radiation.
Venogram is most helpful in making a diagnosis, as it is not too drastic. Only, it has to be done by a special radiologist at a specialist centre.
They can inject the veins with sclerosing agents to block them and they can put little clips inside the veins so that the backward blood flow is stopped. This simple treatment of embolization gives women satisfactory results for several years. The very latest diagnostic and therapeutic technology to manage this condition, treating it effectively with a minimally invasive outpatient procedure.
For those women who cannot avail themselves of the most current and remarkable treatment for PCS
the old medical treatment still helps.
This consists of pain relief by non steroidal antinflammatory medications, oral contraceptive pills, and drugs to suppress the ovaries. Some people believe in Acupuncture, Homeopathic and Osteopathy. Surely all this can be tried with adequate rest and counselling.
In the next post we will talk about Adnexal Pathology (Tubes and Ovaries)
Monday, June 24, 2013
DEEP DYSPAREUNIA
In our previous posts we have been talking about Dyspareunia as apposed to the superficial pain of the vulva, Deep Dyspareunia is caused by deep penetration of the penis into the pelvis.
Deep Dyspareunia is usually due to pelvic pathology and the following conditions are commonly encountered.
1 Endometriosis
2 Adenomyosis
3 Acute and Chronic Pelvic Infections
4 Pelvic Congestion Syndrome
5 Adnexal Pathology
6 Retroverted Uterus
7 Residual Ovary Syndrome
8 Interstitial Cystitis
9 Dry Atrophic Tissues
10 Psychosocial Problems
Endometriosis is a condition, the cause of which we do not understand. In spite of lots of research.
In this condition the lining of the uterus can survive outside the uterus, and with each menstrual cycle has some bleed, as a result of that , some scar tissue forms. Often the blood collects and forms cysts of varying sizes. This can happen at any age group. The main symptom is painful periods, abdominal discomfort, pain on defecation and deep dyspareunia. We talked about clinical history in examination in previous posts but if you are looking for the cause of deep dyspareunia it is important to have an ultrasound and an MRI, so that diagnosis of some of the other conditions can be made.
Endometriosis also causes infertility, the definitive diagnosis is established by a surgical procedure called Laparoscopy, which in simple words mean Key Hole surgery of peeping in the belly.When Endometrios is minor it appears as dark spots which can be lasered or diathermy and this gives relief to the patient. This should be followed by oral contraception, so that the periods are small or none. With this treatment, the chances of endometriosis recurring are minimised. This often helps the women to get pregnant if they were having difficulty.
Diathermy of Endometriotic Implants
during Laparoscopy.
Endometriosis grows under the influence of hormone oestrogen, therefore it grows during reproductive years. It eases off during pregnancy and after menopause. It is a painful condition, the main treatment needs to suppress oestrogens which can be done by many drugs, the simplest being Progesterone and continuous oral contraceptive pill.
The other part of the treatment is pain relief, and this can be done by non steroidal antinflammatory drugs.
If the endometriosis is advanced and has made large cysts , they have to be surgically removed, either by key hole surgery or open surgery. The largest endometriosis I have removed were about the size of two cantaloupes , one on each ovary.
For what ever reason this patient had no pain. The diagnosis was made by Ultrasound.
The youngest patient of endometriosis I have treated with laparoscopic diathermy was thirteen years of age. I was a bit reluctant to do this , but her mother assured me that her pain was very severe and I had to do something.
Endometriosis in itself is a very large topic and needs an individual post which I will do at a later date. But for now, you can remember that this is one of the main causes of Deep Dyspareunia.
Adenomyosis is similar to Endometriosis and here the endometrial implants are within the muscle of the uterus. Month after month there is small bleeding within the muscles of the uterus, as a result the uterus enlarges in size and the patient has heavy and painful periods. She feels as if there is a lump in her belly. When the uterus becomes enlarged it falls backwards, what is called retroverted uterus. This cause chronic pelvic pain and deep dyspareunia. This can also cause pelvic congestion adding to the symptoms. Adenomyosis until recent times was ignored as there were no definitive diagnostic criteria. Recently with the help of colour ultrasound and MRI it has become easy.
There is no definite cure for adenomyosis but we suppress the oestrogens with the pill, intrauterine device called Mirena. The cure is hysterectomy in older women, who do not desire any children and a definitive diagnosis is made when the uterus is in your hand.
The remaining causes of Deep Dyspareunia will be covered in forthcoming posts.
Deep Dyspareunia is usually due to pelvic pathology and the following conditions are commonly encountered.
1 Endometriosis
2 Adenomyosis
3 Acute and Chronic Pelvic Infections
4 Pelvic Congestion Syndrome
5 Adnexal Pathology
6 Retroverted Uterus
7 Residual Ovary Syndrome
8 Interstitial Cystitis
9 Dry Atrophic Tissues
10 Psychosocial Problems
Endometriosis is a condition, the cause of which we do not understand. In spite of lots of research.
In this condition the lining of the uterus can survive outside the uterus, and with each menstrual cycle has some bleed, as a result of that , some scar tissue forms. Often the blood collects and forms cysts of varying sizes. This can happen at any age group. The main symptom is painful periods, abdominal discomfort, pain on defecation and deep dyspareunia. We talked about clinical history in examination in previous posts but if you are looking for the cause of deep dyspareunia it is important to have an ultrasound and an MRI, so that diagnosis of some of the other conditions can be made.
Endometriosis also causes infertility, the definitive diagnosis is established by a surgical procedure called Laparoscopy, which in simple words mean Key Hole surgery of peeping in the belly.When Endometrios is minor it appears as dark spots which can be lasered or diathermy and this gives relief to the patient. This should be followed by oral contraception, so that the periods are small or none. With this treatment, the chances of endometriosis recurring are minimised. This often helps the women to get pregnant if they were having difficulty.
Diathermy of Endometriotic Implants
during Laparoscopy.
Endometriosis grows under the influence of hormone oestrogen, therefore it grows during reproductive years. It eases off during pregnancy and after menopause. It is a painful condition, the main treatment needs to suppress oestrogens which can be done by many drugs, the simplest being Progesterone and continuous oral contraceptive pill.
The other part of the treatment is pain relief, and this can be done by non steroidal antinflammatory drugs.
If the endometriosis is advanced and has made large cysts , they have to be surgically removed, either by key hole surgery or open surgery. The largest endometriosis I have removed were about the size of two cantaloupes , one on each ovary.
For what ever reason this patient had no pain. The diagnosis was made by Ultrasound.
The youngest patient of endometriosis I have treated with laparoscopic diathermy was thirteen years of age. I was a bit reluctant to do this , but her mother assured me that her pain was very severe and I had to do something.
Endometriosis in itself is a very large topic and needs an individual post which I will do at a later date. But for now, you can remember that this is one of the main causes of Deep Dyspareunia.
Adenomyosis is similar to Endometriosis and here the endometrial implants are within the muscle of the uterus. Month after month there is small bleeding within the muscles of the uterus, as a result the uterus enlarges in size and the patient has heavy and painful periods. She feels as if there is a lump in her belly. When the uterus becomes enlarged it falls backwards, what is called retroverted uterus. This cause chronic pelvic pain and deep dyspareunia. This can also cause pelvic congestion adding to the symptoms. Adenomyosis until recent times was ignored as there were no definitive diagnostic criteria. Recently with the help of colour ultrasound and MRI it has become easy.
There is no definite cure for adenomyosis but we suppress the oestrogens with the pill, intrauterine device called Mirena. The cure is hysterectomy in older women, who do not desire any children and a definitive diagnosis is made when the uterus is in your hand.
The remaining causes of Deep Dyspareunia will be covered in forthcoming posts.
Monday, June 10, 2013
VULVODYNIA
In my previous blog we talked about Rena's story when her honeymoon became a disaster.
We talked about the reasons and their management.
Today we have a similar story about Ashley, due to another cause of Vulval pain.
This is called Vulvodynia. She has been having this painful condition for almost a year, her social and marital life is very strained and stressed and she is already seeing two clinicians without any satisfactory resolution.
Vulvodynia was described for the first time in 1880. It was already mentioned in my previous post as Super Sensitivity of the Vulva. However it was ignored almost for a hundred years, then in 1975 International Society of Vulvo Vaginal Diseases, called it Burning Vulval Syndrome.
It is a very poorly recognised female pain disorder although one in four women suffer it sometime during their lifespan from adolescence to post menopause.
The current definition of Vulvodynia by ISSVD is:
"Chronic Vulval discomfort, most often described as burning pain, occurring in the Absence of relevant visible findings or a specific, clinically identifiable, neurological disorder"
We do not yet understand the full story of Vulvodynia.
Misdiagnosis is the commonest cause of suffering, when only one point four percent seeking medical advise are correctly diagnosed. It affects the quality of life , the women get confused, there is delay in treatment and they self medicate.
Vulvodynia can be generalised , that means that it is all over the vulva, or it can be localised, the most common sites are the vestibule and the clitoral area.
And then it is called Vulvo Vestibulitis or Clitoral Vestibulitis.
When a patient comes to you with vulval pain , you take a detailed history, of how long she has had the pain,and the events that started the pain.
Sexual activity can it be continued and Psycho Sexual relationships with her partner. It is also worthwhile to know if she has had any operation in that area, and has she had a child.
The hygiene practices are also important to know.
On examination , we should inspect the vulva, look for any ulcers, scarring and muscle spasms, called vaginismus.
We take swabs, skin scrapings, and cervical cytology to exclude any other diseases.
One of the very simple tests is to give a cotton wool swab to the patient and ask them to show where the pain is most.
The three criteria for the diagnosis of vulvodynia , is very mild pain on touch, no positive findings and mild redness of the vulva. There are very little minor glands in the vestibule that get inflamed and cause pain.
The vulvodynia can be classified into three categories : One is the intercourse despite being painful that can be carried out with some degree of discomfort. Second Category has to be discontinued due to pain and the Third is sex cannot happen.
Vulvodynia was primarily thought to be psycho sexual but we think that there is neural problems, these most often resolve in time.
Treat any existing problems that you may have come across during your investigation.
The explanation of the condition given to the patient and the reassurance that about seventy five percent can be treated helps them.
The general advice should emphasis is that they should not self medicate and get a clear cut diagnosis.
They can wash themselves with a freshly prepared saline solution consisting of two teaspoons of salt in a litre of water. They can use cold packs to relieve the pain, do not use commercial perfumes or antiseptics and wear light clothing. Try and improve your relationships and relieve the stress.
Follow the treatment for vaginismus , you may need help of a physiotherapist who is happy to give you bio feed back treatment. Electromagnetic treatment has been tried.
Neurological Antidepressants such as Amitriptyline with a small starting dose of 10mgs. It is thought to act as nerve membrane stabiliser.
Local lubricants (water based) are useful, oestrogen cream is useful in peri menopausal women.
Five percent Xylocaine cream can be applied at the time of intercourse.
Surgically vestibulectomy has been tried with significant improvement.
Now because we think that there is a neurological involvement we are doing more studies on the refining the diagnostic criteria and treatment of this very elusive condition.
The various other Vulvo Vaginal problems will be discussed in future posts.
We talked about the reasons and their management.
Today we have a similar story about Ashley, due to another cause of Vulval pain.
This is called Vulvodynia. She has been having this painful condition for almost a year, her social and marital life is very strained and stressed and she is already seeing two clinicians without any satisfactory resolution.
Vulvodynia was described for the first time in 1880. It was already mentioned in my previous post as Super Sensitivity of the Vulva. However it was ignored almost for a hundred years, then in 1975 International Society of Vulvo Vaginal Diseases, called it Burning Vulval Syndrome.
It is a very poorly recognised female pain disorder although one in four women suffer it sometime during their lifespan from adolescence to post menopause.
The current definition of Vulvodynia by ISSVD is:
"Chronic Vulval discomfort, most often described as burning pain, occurring in the Absence of relevant visible findings or a specific, clinically identifiable, neurological disorder"
We do not yet understand the full story of Vulvodynia.
Misdiagnosis is the commonest cause of suffering, when only one point four percent seeking medical advise are correctly diagnosed. It affects the quality of life , the women get confused, there is delay in treatment and they self medicate.
Vulvodynia can be generalised , that means that it is all over the vulva, or it can be localised, the most common sites are the vestibule and the clitoral area.
And then it is called Vulvo Vestibulitis or Clitoral Vestibulitis.
When a patient comes to you with vulval pain , you take a detailed history, of how long she has had the pain,and the events that started the pain.
Sexual activity can it be continued and Psycho Sexual relationships with her partner. It is also worthwhile to know if she has had any operation in that area, and has she had a child.
The hygiene practices are also important to know.
On examination , we should inspect the vulva, look for any ulcers, scarring and muscle spasms, called vaginismus.
We take swabs, skin scrapings, and cervical cytology to exclude any other diseases.
One of the very simple tests is to give a cotton wool swab to the patient and ask them to show where the pain is most.
The three criteria for the diagnosis of vulvodynia , is very mild pain on touch, no positive findings and mild redness of the vulva. There are very little minor glands in the vestibule that get inflamed and cause pain.
The vulvodynia can be classified into three categories : One is the intercourse despite being painful that can be carried out with some degree of discomfort. Second Category has to be discontinued due to pain and the Third is sex cannot happen.
Vulvodynia was primarily thought to be psycho sexual but we think that there is neural problems, these most often resolve in time.
Treat any existing problems that you may have come across during your investigation.
The explanation of the condition given to the patient and the reassurance that about seventy five percent can be treated helps them.
The general advice should emphasis is that they should not self medicate and get a clear cut diagnosis.
They can wash themselves with a freshly prepared saline solution consisting of two teaspoons of salt in a litre of water. They can use cold packs to relieve the pain, do not use commercial perfumes or antiseptics and wear light clothing. Try and improve your relationships and relieve the stress.
Follow the treatment for vaginismus , you may need help of a physiotherapist who is happy to give you bio feed back treatment. Electromagnetic treatment has been tried.
Neurological Antidepressants such as Amitriptyline with a small starting dose of 10mgs. It is thought to act as nerve membrane stabiliser.
Local lubricants (water based) are useful, oestrogen cream is useful in peri menopausal women.
Five percent Xylocaine cream can be applied at the time of intercourse.
Surgically vestibulectomy has been tried with significant improvement.
Now because we think that there is a neurological involvement we are doing more studies on the refining the diagnostic criteria and treatment of this very elusive condition.
The various other Vulvo Vaginal problems will be discussed in future posts.
Thursday, May 30, 2013
DYSPAREUNIA OR WHEN SEX HURTS
DYSPAREUNIA OR WHEN SEX HURTS
Pretty girl Rena came to see me in my office upon return from her honeymoon, she was in tears, this honeymoon was a total disaster, as they could not enjoy or have any sexual entertainment or pleasure.
Dyspareunia means painful sex, and the word is derived from Greek, which means (Badly Mated).
When you cannot have sex at all is called Apreunia.
Vulval pain is in fact quite a common condition, more often occurring in women, almost one in four women suffer with Dyspareunia during there life span.
Historically it was described in 1880 as hypersensivity or super sensitivity of the vulva. It was in 1975 that the Vulvovaginal Disease Society gave it a name , burning vulva syndrome.
We have come a long way in understanding the problem , however we do not totally understand what causes it. In the past the condition was considered to be psychological, however luckily for the modern women the current diagnostic and therapeutic approach is integrated with some psychology.
Dyspareunia is a complex problem and frequently has a multifactorial aetiology. A new way has been recently suggested to define dyspareunia by dissecting it into primary, secondary, and tertiary sources of pain. It is also defined into superficial or deep depending on the origin of the pain and these will be discussed in future blogs.
We are talking about pain in the female external genitalia which lies between our thighs, and it is called the Vulva.
The picture shows all the female genital organs. The vulva consists of Labia Majora on both sides and in side this is Labia Minora on both sides. On the top is the Urethra and just above is the Clitoris not seen in the diagram. The little opening leads to the Vagina and the area around is called the vestibule. It is in this area that the pain is called Dyspareunia.
As a result of the pain the muscles of the area go into a spasm, and this is then called vaginismus.
Vaginismus can often happen before the sex is initiated, due to fear or psychological reasons.
Dyspareunia can be superficial, due to the visible structures or deep within the vaginal area.
In this post we will concentrate on some of the superficial causes of pain. We will not talk about the skin conditions, such as infections, dermatitis, herpes, human papilloma virus, congenital abnormalities such as the vaginal septum's, tough hymen, absent hymen or even absent vagina. Hymen is a membrane with a small opening in the centre , through, which the menstrual blood flows. At the time of commencement of sexual activity, the penis goes through the hymen, enlarging the opening.
Sometimes if this is not possible a medical procedure is necessary to enlarge it.
This type of difficulty along with painful infections or fear, disparity between the size of the mans penis and vagina, the vulva goes into a muscular spasm, this is very painful and some times extends into the women's legs.
Women coming from very conservative families , lack of education and abuse as a child, along with
local operations on the vulva and traumatic child birth, also get vaginismus.
So as medical practitioners after taking a detailed history and clinical examination should then advise the treatment accordingly.
The simplest thing to start with is to give basic education on sexual intercourse, reassurance, and some antidepressants.
Physiotherapy of the pelvic floor is useful.
It the vaginismus is not to severe you can help, by teaching the patient how to dilate the vagina. The vagina should be well lubricated, watery lubricants should be used. In my experience I have found Olive Oil to be a very good lubricant. The women should avoid using off the counter preparations, such as strong soaps, talcum powder or perfumes. The best thing to wash is with plain clean water.
The dilators are available as a set of gradually increasing size and the women can lubricate it slowly in the shower.
In very severe cases of vaginismus where the sex is totally impossible the treatment has to be taken.
One of the best treatments was described by Master and Johnson in 1970, still makes great sense to me. There advise that the couple should have a peaceful time to have relationship, initially they should touch each on non sexual organs, taking it in turns as to who starts first. There is total ban on sexual activity until the women is totally relaxed. There should be a fair bit of foreplay until she is well lubricated. The sexual activity should start with regular gentle stretching.
This condition is almost always reversible.
The next important condition causing superficial Dyspareunia is currently named Vulvodynia and we will talk about this in the next blog.
Pretty girl Rena came to see me in my office upon return from her honeymoon, she was in tears, this honeymoon was a total disaster, as they could not enjoy or have any sexual entertainment or pleasure.
Dyspareunia means painful sex, and the word is derived from Greek, which means (Badly Mated).
When you cannot have sex at all is called Apreunia.
Vulval pain is in fact quite a common condition, more often occurring in women, almost one in four women suffer with Dyspareunia during there life span.
Historically it was described in 1880 as hypersensivity or super sensitivity of the vulva. It was in 1975 that the Vulvovaginal Disease Society gave it a name , burning vulva syndrome.
We have come a long way in understanding the problem , however we do not totally understand what causes it. In the past the condition was considered to be psychological, however luckily for the modern women the current diagnostic and therapeutic approach is integrated with some psychology.
Dyspareunia is a complex problem and frequently has a multifactorial aetiology. A new way has been recently suggested to define dyspareunia by dissecting it into primary, secondary, and tertiary sources of pain. It is also defined into superficial or deep depending on the origin of the pain and these will be discussed in future blogs.
We are talking about pain in the female external genitalia which lies between our thighs, and it is called the Vulva.
The picture shows all the female genital organs. The vulva consists of Labia Majora on both sides and in side this is Labia Minora on both sides. On the top is the Urethra and just above is the Clitoris not seen in the diagram. The little opening leads to the Vagina and the area around is called the vestibule. It is in this area that the pain is called Dyspareunia.
As a result of the pain the muscles of the area go into a spasm, and this is then called vaginismus.
Vaginismus can often happen before the sex is initiated, due to fear or psychological reasons.
Dyspareunia can be superficial, due to the visible structures or deep within the vaginal area.
In this post we will concentrate on some of the superficial causes of pain. We will not talk about the skin conditions, such as infections, dermatitis, herpes, human papilloma virus, congenital abnormalities such as the vaginal septum's, tough hymen, absent hymen or even absent vagina. Hymen is a membrane with a small opening in the centre , through, which the menstrual blood flows. At the time of commencement of sexual activity, the penis goes through the hymen, enlarging the opening.
Sometimes if this is not possible a medical procedure is necessary to enlarge it.
This type of difficulty along with painful infections or fear, disparity between the size of the mans penis and vagina, the vulva goes into a muscular spasm, this is very painful and some times extends into the women's legs.
Women coming from very conservative families , lack of education and abuse as a child, along with
local operations on the vulva and traumatic child birth, also get vaginismus.
So as medical practitioners after taking a detailed history and clinical examination should then advise the treatment accordingly.
The simplest thing to start with is to give basic education on sexual intercourse, reassurance, and some antidepressants.
Physiotherapy of the pelvic floor is useful.
It the vaginismus is not to severe you can help, by teaching the patient how to dilate the vagina. The vagina should be well lubricated, watery lubricants should be used. In my experience I have found Olive Oil to be a very good lubricant. The women should avoid using off the counter preparations, such as strong soaps, talcum powder or perfumes. The best thing to wash is with plain clean water.
The dilators are available as a set of gradually increasing size and the women can lubricate it slowly in the shower.
In very severe cases of vaginismus where the sex is totally impossible the treatment has to be taken.
One of the best treatments was described by Master and Johnson in 1970, still makes great sense to me. There advise that the couple should have a peaceful time to have relationship, initially they should touch each on non sexual organs, taking it in turns as to who starts first. There is total ban on sexual activity until the women is totally relaxed. There should be a fair bit of foreplay until she is well lubricated. The sexual activity should start with regular gentle stretching.
This condition is almost always reversible.
The next important condition causing superficial Dyspareunia is currently named Vulvodynia and we will talk about this in the next blog.
Monday, April 8, 2013
OSTEOPOROSIS
Osteoporosis is a very common condition in the present world , perhaps because we are living longer. Osteoporosis in simple language means fragile bones. It is more common in females. One in Five females suffer from this after the age of fifty, the recent study done in Australia showed that there were 1.3 million osteoporotic women in Australia compared with 50 million women in USA in 2010. 80 thousand women each year in Australia, suffer from a fracture from minor trauma, usually in the arm , hip and spine.
Billions of dollars are spent on health budgets to look after these women and men.
And the misery they suffer from the complications are immeasurable.
Osteoporosis is a preventable disease and we can save so much pain and suffering and cost if we act early.
This prevention really should be started in childhood, its like the foundation of a house, the better , the longer the house will stand. Like the repair of the house , the body also needs constant care to prevent osteoporosis.
The four important factors that are adequate nutrition, calcium, vitaminD and physical activity.
In very young children up to the age of 4 you need 500mgs of calcium per day, then in adolescents about 700mgs and teenagers about 1000mgs. In older women the need increases again to 1300mgs per day.
Five to ten minutes of sport in the sun each day is enough to keep their vitamin d levels up to around 50units.
So as you can see it is very simple to maintain your bone health.
The best bone health is around late twenty's and it is called peak bone mass.
So if you have your best bone density at that age, your risk of osteoporosis is 30% less in old age.
There are some risk factors which increase the risk of osteoporosis , the most important being genetics, a frail figure, smoking, long term use of steroids, for example in Asthma, early menopause, poor gonadal activity(poor development).
The diagnosis is best made by bone density scan, called "dexa scan".
More tests are performed in complicated cases to study the calcium metabolism, and hormones involved in bone formation.
The treatment is simple, keep your calcium, Vitamin D and exercise up.
The drugs required fall in to two categories' one is to stop the bone destruction, and the other is to make the bones remodel. The bones get repaired all the time by the process of absorption and remodelling .
Hormone replacement in women is the best treatment for prevention and management of osteoporosis, except where this cannot be given.
It is very useful to take HRT in early menopause preferably before the age of sixty.
DO NOT BE AFRAID of HRT or MHT, do not suffer and enjoy life.
There are many other drugs available, for the management of osteoporosis, and they fall under the group of drugs called anti absorptive, they are called Bisphonates.
Nothing is worse than lying in a hospital with a broken hip, hanging in a sling, counting days, don't let it happen, do not be anti HRT, you cannot treat osteoporosis by calcium , vitamin d only.
To build a house you need a builder which is the HRT and you need concrete which is Calcium and Vitamin D.
Monday, April 1, 2013
"HOT FLASHES"
Timing is everything in managing them. So how old are you today?. and you couldn't sleep all night yesterday because of them. So now is the right time to start HRT (Hormone Replacement Therapy), take the real diamond (the proper commercial drug) not naturopathic or homeopathic. They have not been scientifically tested and they do not really help.
While all HRT carries some risks, but they are very useful in giving you a new lease of life, no hot flashes, good sleep, and happy sexual interludes.
It prevents the long term side affects of menopause such as Osteoporosis , Bladder control, and newly diagnosed Diabetes. If you are between 45 and 60, now is the best time to start to enjoy life.
See a doctor who is familiar with all forms of HRT and have it tailored to your needs.
Use of custom-compounded bio identical therapy is not recommended.
Special care has to be taken if there is risk of venous thromboembolism, stroke, ischemic, heart disease. The risk of breast cancer in women over fifty years is a complex issue and needs very special attention.
In women with premature or surgical menopause HRT, should be given up to the age of normal menopause.
There is a lot more to menopause than this brief summary. DO NOT BE AFRAID of HRT or MHT, do not suffer and enjoy life.
Subscribe to:
Comments (Atom)